Title: Community in Crisis: The Impact of Providence’s Closure of Adolescent Psychiatric Unit in Spokane
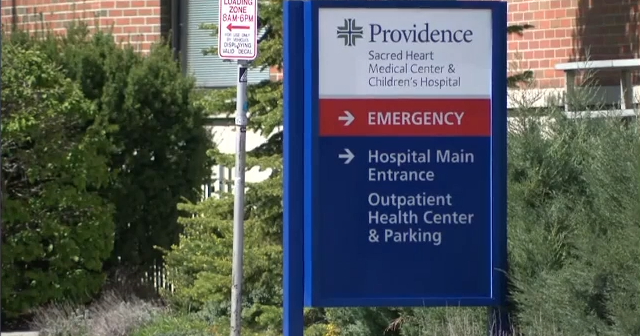
In the heart of Spokane, Washington, a significant healthcare decision is stirring concern among local families and mental health advocates. Providence Sacred Heart Medical Center recently announced the closure of its adolescent inpatient psychiatric unit, claiming that this move will not adversely affect the community’s mental health services. However, the Washington State Nurses Association (WSNA) is taking a firm stand against this assertion, labeling it misleading and indicative of a deeper issue within the region’s mental health framework.
A Closer Look at the Closure
Providence’s decision, initially framed as a necessary step due to financial constraints, has sent shockwaves through a community already grappling with mental health challenges. The WSNA, representing professionals who work closely with vulnerable youth, highlighted that although some inpatient services remain available in the area, the closure of this specialized unit significantly diminishes the level of care for adolescents experiencing mental health crises.
The Providence unit was unique in its ability to address complex cases involving not just mental health issues, but also co-occurring medical conditions. For instance, adolescents with insulin-dependent diabetes, autism, or developmental delays found a critical support system in this facility. These complexities mean that not all facilities are equipped to handle such cases, with many turning away patients who desperately need help. The reduction in specialized care can lead to increased hospitalizations elsewhere or, worse, a lack of necessary care altogether.
Layoffs and the Ripple Effect
Adding to concerns surrounding the psychiatric unit’s closure are the layoffs that took place in December 2022. Eight physicians were let go as part of a cost-saving effort and restructuring plan, a move that the hospital initially promised to rectify by restoring these positions. However, since then, the number of patients served has dwindled, and uncertainty about future contracts for healthcare providers has further complicated recruitment efforts. This gap in psychiatric care could leave families facing a daunting search for the right facilities for their children.
Financial Claims Under Scrutiny
While Providence argues that financial limitations are forcing the closure, critics have pointed out an incongruity in their narrative. The nonprofit hospital holds a 20% stake in Inland Behavioral Health, a facility operated by the for-profit entity Universal Health Services. This investment raises questions about how Providence is allocating its resources and whether there are alternative solutions available to avoid such drastic cuts to essential services.
Moreover, an analysis of the regional mental health landscape indicates that Inland Northwest Behavioral Health does accept patients aged 13 to 17, at odds with Providence’s claim that it serves primarily 12-year-olds. This discrepancy highlights a pressing need for greater transparency around the hospital’s claims concerning patient care capabilities and the implications of its closure.
Voices from the Community
In light of these developments, the WSNA has voiced deep concern for the adolescents and families who depended on the specialized services of the Sacred Heart unit. The association stresses that when treatment options are reduced, vulnerable populations are disproportionately affected, leading to worse patient outcomes and potentially skyrocketing healthcare costs in the long term.
Community advocates, parents, and healthcare professionals alike are urging Providence to reconsider its decision and find alternative strategies to support its financial viability without sacrificing essential mental health services. As mental health issues continue to rise, particularly in the wake of the COVID-19 pandemic, the role of such specialized treatment facilities is more critical than ever.
The Path Forward
Spokane is at a crossroads, facing a mental health care dilemma that could set a precedent for how local hospitals address financial challenges in the future. The closure of the adolescent psychiatric unit raises urgent questions about access to care, prioritization of community health, and the responsibilities of nonprofit organizations to the populations they serve.
As the community grapples with these complex issues, it becomes increasingly clear that a collaborative approach—one that brings together healthcare providers, policymakers, and families—is essential. The well-being of Spokane’s youth hangs in the balance, and it is imperative that all stakeholders come together to ensure that no child is left without the care they need.
As the story unfolds, residents are left to ponder whether Providence can align its financial strategies with the pressing mental health needs in Spokane, or if other alternatives should be pursued to safeguard the health and well-being of the community’s most vulnerable population.


:quality(70)/cloudfront-us-east-1.images.arcpublishing.com/shawmedia/CJP5DWVY3FAO3O3NBYHNAXSH64.jpg)